Pediatric Hand Disorders- All you need to know

Nutritional Requirements in Growing Children
November 26, 2020
Understanding the Importance of Bone Health during COVID 19
December 19, 2020
Pediatric hand disorders are finger or hand deformities that occur at birth. Any form of deformity in a new-born becomes a challenge for the child as they begin to grow. Hand deformities can especially disable the child as they learn to engage with the environment with their hands’ help.
The degree of deformity differs from a minor deformity, like unequal, uneven thumb or finger deformity, to a severe deformity, like the complete absence of a bone.
Here are some of the most common pediatric hand deformities:
1. Polydactyly
Polydactyly is a condition in which the child is born with one or more extra fingers or toes. It can occur on one or both hands or feet.
Polydactyly varies in the way it presents itself. It can appear as:
- A small, raised lump of soft tissue, having no bones (known as nubbin)
- Partially formed finger containing few bones but no joints
- Completely functioning finger with bones, tissues, and joints
There are three primary forms of polydactyly:
- Ulnar or postaxial polydactyly or small finger duplication: This is the most known version of the condition. An additional finger is on the outside of the little finger of the child. Such a side of the hand is called the ulnar side.
- Radial or preaxial polydactyly or thumb duplication: This condition is not that common, taking place in 1 in each 1,000 to 10,000 live births. The child’s extra finger is on the outside of the thumb. This side of the hand is called the radial side.
- Central polydactyly: This is a rare form of polydactyly. The child’s extra finger is attached to the ring, middle, or commonly on the index finger.
Causes of Polydactyly
Polydactyly can be passed down in families. A passed down polydactyly is called familial polydactyly. This kind of polydactyly happens in isolation. It means the child may not have any associated symptoms.
Polydactyly can also be linked with a genetic condition, which means it can be passed down along with a genetic condition. If polydactyly is not passed down, it happens because of a change in the child’s genes while it is in the womb.
Some kinds of polydactyly are more likely to be passed down. Others are more likely to be linked with a genetic condition.
Treatment for Polydactyly
Treatment depends on the type of condition the child has:
Small finger duplication
The child may not require small finger duplication treatment because it does not affect how they will use their hand.
Thumb duplication
Treatments for thumb duplication are more complex as the additional thumb may affect the child’s other thumb’s working.
For this reason, it is not possible to remove the extra thumb. Surgery is required to reconstruct one working thumb, using parts of both thumbs.
Central polydactyly
Central polydactyly can progress to a complete-functioning extra finger. In such a condition, removal may be required. Removal is needed only if one desires the digit to be removed.
2. Syndactyly
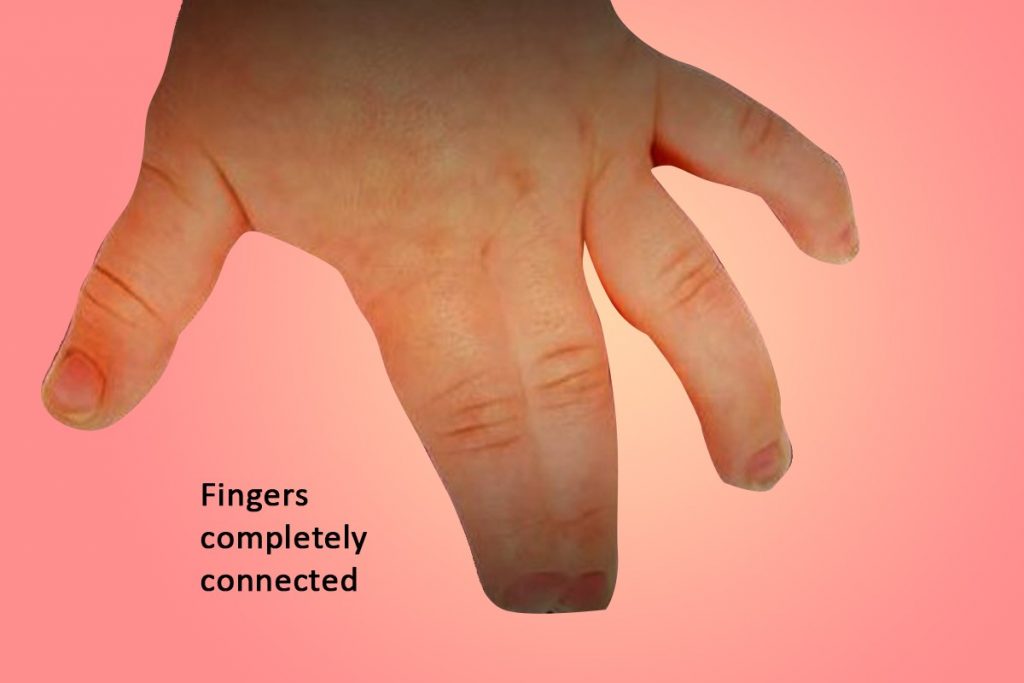
Syndactyly is the unnatural link between the child’s two fingers. Most commonly, it is the webbing between the child’s ring and middle fingers. That said, it can include any two of the child’s fingers or consist of the thumb and pointer finger. In some cases, it involves more than two fingers.
Webbing consists of the child’s entire two fingers or a part of the fingers. It can be the child’s skin or can involve the bone as well.
There are three forms of Syndactyly:
Partial vs. complete syndactyly: It involves a part of the child’s fingers (partial) or the complete fingers (to the tip)
Cutaneous vs. complex syndactyly: Cutaneous (or “simple”) syndactyly shows only a skin connection. Complex syndactyly involves bony interconnections between the child’s fingers.
Complicated syndactyly: Syndactyly has a connection with a syndrome (often a condition with other health issues).
Function and Appearance
Usually, children with syndactyly function well, without the need for any treatment. However, the more fingers that are affected, the more difficult function can be.
The syndactyly’s primary functional issues are grabbing big objects or holding circular objects (as the child’s fingers do not spread apart). The appearance of the child’s hand is different with syndactyly. It can disturb a child and can change the way others relate with the child. In some kids, this can cause stress and reduce self-esteem.
Treatment for Syndactyly
The only way to correct syndactyly is through surgery. The timing of surgery is based on several different factors. When syndactyly affects the child’s thumb and pointer finger or ring and small finger, surgery can occur early by 6 months. When the child is older, other syndactylies can be treated, usually between 12 and 18 months.
3. Pediatric Trigger Thumb (PTT)
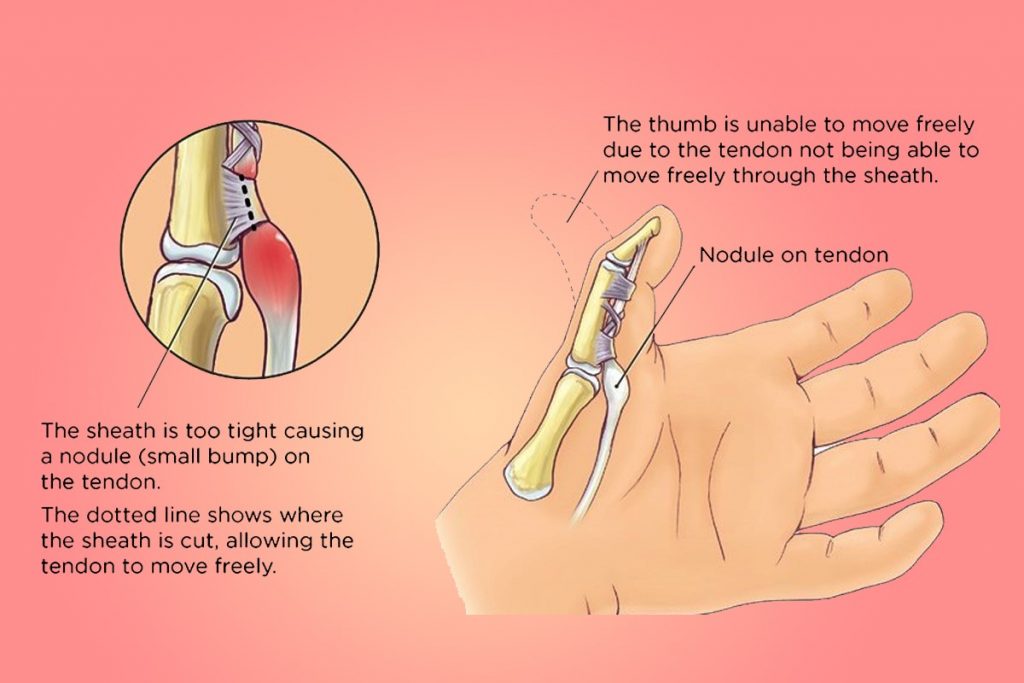
Pediatric trigger thumb (PTT) is also known as flexion contracture of the IP joint. It is a condition that can affect the movement of the thumb in the child. The thumb gets stuck in a bent position. A contracture means that a child’s thumb can no longer straighten or longer stretch.
Tendons work to make thumbs move. They act like strings within the thumb and are held in place with the tunnel system of ligaments (also called “pulleys”).
Such ligaments or tunnels keep the tendon near a bone and permit it to slide back and forth. When the tendons are pulled through the ligament, the thumb flexes or bends.
In PTT, a tendon cannot perform the same procedure. The child’s thumb gets restricted in a flexed position. They cannot straighten their thumb. The name “trigger” is from the clicking sensation. This clicking sensation occurs when the tendon pops through the ligament. Also, when the tendon “triggers” between a restricted position and a straight position.
Cause of Pediatric Trigger Thumb
What causes PTT is not known. Kids are not born with it. It does not happen due to overuse, injury, or trauma.
However, because of the mismatch in the tendon and ligament sizes, the ligament becomes too tight on the tendon. It causes the tendons to swell and become thick. Sometimes a bump, known as Notta’s nodule, occurs on the tendon. The Notta’s nodule prevents the tendons from gliding correctly.
About 3 in 1000 children can get a PTT between ages 1 and 3. It often develops in children when they are about 2 years old. Boys and girls are at the same risk of developing PTT. Both thumbs may be affected in up to 30 percent of children.
Treatment for Pediatric Trigger Thumb
There are three methods to treat PTT.
Wait and watch to check if the child’s flexion contracture disappears on its own: In children younger than one year of age, PTT can disappear without anything any treatment. It may require many months or years.
Stretching and splinting your thumb: A pediatric orthopedic will teach how to massage and stretch the child’s thumb. After stretching, the thumb will be kept straight in a splint. The child may require wearing a splint all the time or at specific times, like when sleeping. Keeping the thumb in a straight position without permitting any movement can help reduce the swelling.
Surgery: If PTT does not disappear on its own and splinting and stretching does not work, surgery can heal the issue.
When to see a Doctor?
Parents can consult a doctor for treatment to enhance the child’s ability to function with a hand disorder. Another goal is to better the appearance of the hand and support the child’s self-esteem.
Every child with a hand disorder is different. So, the treatment approach depends on a child’s requirements.
Note that treatment cannot “cure” a hand disorder. However, it can help to improve the function and appearance of the child’s hand.
A positive attitude and accepting the difference – by the child and the parents – are vital to treatment success and healthy development.