Perthes Disease – All you need to know

A 9-Year-Old with Left Foot Deformity Treated with Corrective Surgery
May 18, 2021
Congenital Short Femur – All you need to know
May 21, 2021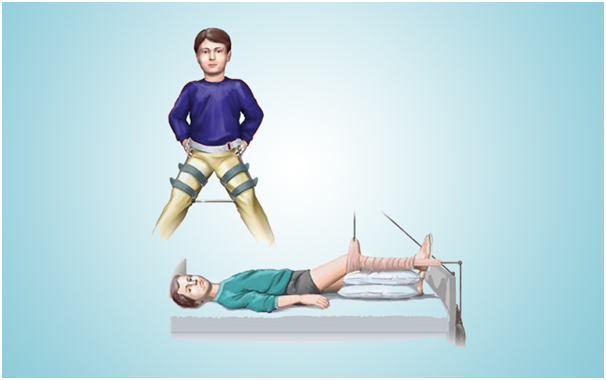
Perthes disease, also known as Legg-Calve-Perthes, affects children between the ages of four and ten. While it is five times more common in boys than in girls, it is more likely to cause bone damage in girls. Both hips are affected in ten percent to fifteen percent of all cases. The cause of Perthes disease is not known. So, parents must visit a pediatric orthopedic doctor in Gurgaon for proper diagnosis and treatment.
Perthes disease is divided into four stages:
- Necrosis:
During this stage, the blood flow to the head of the femur is compromised, and bone cells die. The affected area will become inflamed or irritated. Also, the child will begin to show symptoms of the disease, including limping and differences in walking. This preliminary stage could last for many months.
- Fragmentation:
The body removes the dead bone underneath the articular cartilage and quickly replaces it with a new, softer bone within a period of 1 to 2 years. The bone is weaker during this process, and the femur head might fall into a flatter position.
- Reossification:
In the head of the femur, new, stronger bone forms and takes shape. The reossification stage of the disease is always the longest, lasting many years.
- Healed:
The bone regrowth is completed at this stage, and it starts to take shape in the head of the femur. The extent of damage during the fragmentation process, and the child’s age at the onset of disease, determines how similar the shape is to round. These factors also affect the potential for bone regrowth.
What are the symptoms of Perthes disease?
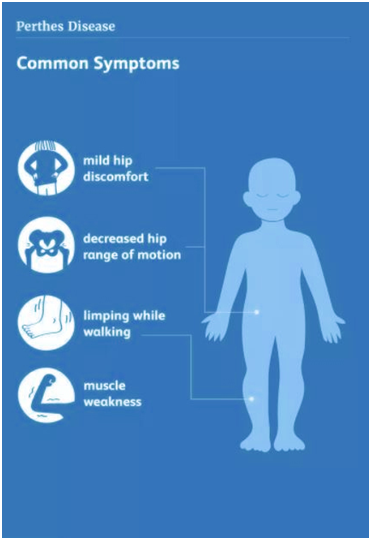
A shift in the child’s walking and running style is one of the first symptoms of Perthes. This is most noticeable when participating in sports. The child can limp, have limited motion, or develop an unusual running style because of irritability in the hip joint.
Some other symptoms include:
- Pain in the hip or groin, and other areas of the leg, such as the thigh or knee
- Pain that gets worse with activity and relieves with rest.
- Painful muscle spasms because of irritation near the hip
Symptoms can come and go over weeks or even months, depending on the child’s activity level.
How is Perthes disease treated?
Perthes disease can be treated in several ways.
Treatment of Perthes disease aims to alleviate painful symptoms, preserve the femoral head’s shape, and restore hip movement.
The pediatric orthopedic specialist will consider the following factors when formulating a treatment plan for a child,
- The child’s age: Younger children (those under the age of six) have a better chance of developing new, healthy bones.
- The extent of damage to the femoral head: If necrosis has affected more than half of the femoral head, the chances of bone regrowth without deformity are low.
- The child’s disease stage at the time of diagnosis: The treatment option recommended by a pediatric orthopedic specialist is determined by the stage at which the child is during the disease’s diagnosis.
- Depending on the above factors a pediatric orthopedic specialist may recommend nonsurgical or surgical treatment options.
- If the condition is left untreated, the femoral head will lose its shape and no longer fit inside the acetabulum, causing hip problems later in life, such as early-onset arthritis.
Nonsurgical treatment
- Observation:
Young children (2 to 6 years old) with some changes in the femoral head on their initial x-rays are kept on observation. The pediatric orthopedic specialist will use x-rays to regularly examine the child. It will ensure that the bone regrowth is progressing smoothly.
- Anti-inflammatory medicines
Inflammation of the hip joint causes painful symptoms. Anti-inflammatory medications, such as ibuprofen, are used to relieve pain and can be prescribed by the pediatric orthopedic specialist for some time. The pediatric orthopedic specialist will change the dose or stop the medication as the child progresses through the stages of the disease.
- Limiting activities
Running and jumping are high-impact movements that should be avoided to alleviate pain and protect the femoral head. To prevent the child from placing too much weight on the joint, the pediatric orthopedic specialist may recommend a walker or crutches.
- Physical therapy
In children with Perthes disease, hip stiffness is common. Physical therapy exercises are recommended to help restore the range of motion of the child’s hip joint. These exercises usually focus on hip abduction and internal rotation.
Surgical treatment
A pediatric orthopedic specialist may recommend surgery to re-align the bones of the hip and hold the femur head deep inside the acetabulum until the healing process is complete. Surgery is recommended when:
- A child is older than 8 years old at the time of diagnosis. Preventing damage to the femoral head is more important in older children because the risk of deformity during the reossification stage is higher.
- More than half of the femoral head has been damaged. Keeping the femoral head inside the rounded acetabulum can help the bone develop into an afunctional shape.
- Nonsurgical treatment has not held the hip in the correct place for healing.
An osteotomy is the most common surgical technique used to treat Perthes disease. Under this procedure, the bone is cut and repositioned to hold the femoral head inside the acetabulum. This alignment is held with screws and plates, which will be removed after the healed stage of the disease.
In most cases, children with Perthes have a good long-term prognosis and grow without further hip problems.
If there is a remaining deformity in the shape of the femoral head, there is a higher risk of possible complications in the future. Hip pain or arthritis in adulthood will develop when the deformed femoral head does not fit well into the acetabulum.