Mucopolysaccharidoses Treatment in Gurgaon, Delhi NCR
Dr.Ratnav Ratan is an expert pediatric orthopaedic surgeon in Gurgaon and Delhi NCR offering comprehensive treatment of orthopaedic disorders due to mucopolysaccharide in infants and growing children. These children exhibit skeletal abnormalities such as hip dysplasia, genu valgum,thoracic kyphosis and proportionate dwarfism, and so on very early and hence suitable medical intervention is advisable without further delay.
What are Mucopolysaccharidoses
Mucopolysaccharidoses are a set of genetic metabolic diseases defined by the excretion of mucopolysaccharide (sugar) in the urine. These diseases include:
- MPS I – Hurler:MPS I or Hurler is caused when the enzyme alpha-L-iduronidase is absent or present in inadequate amounts. The faulty gene is passed along to children born to MPS I parents.
- MPS II – Hunter: The lack of the enzyme iduronate sulfatase or iduronate sulfatase deficiency causes MPS II, Hunter syndrome. It is the only mucopolysaccharidoses in which the faulty gene can be passed to a son by the mother alone (due to X-linked recessive inheritance).
- MPS III – Sanfilippo:Sanfilippo syndrome, also known as MPS III, is characterised by severe neurological abnormalities. It is caused by the alteration of a different enzyme needed to completely break down the heparan sulphate sugar chai
- MPS IV – Morquio: MPS IV, also known as Morquio syndrome occurs when the enzymes N-acetylgalactosamine-6-sulfatase (GALNS) and beta-galactosidase required to break down the keratan sulphate sugar chain are missing or defective.
- MPS VI – Maroteaux–Lamy: MPS VI, also known as Maroteaux–Lamy syndrome,is caused by the deficiency of enzyme N-acetylgalactosamine 4-sulfatase.
Symptoms can be similar or different depending on the type of disease and improvements in the patient’s condition can be made by an orthopedic doctor in Gurgaon. Most of these diseases are recessive, meaning they are passed down from both parents, and therefore are difficult to diagnose at birth and during the child’s first year.
The condition is caused by the body’s inability to break down mucopolysaccharides (long chains of sugar moleculesfound throughout the body).
Patients with mucopolysaccharidosisdo not make enough enzymes to convert these sugar chains into proteins and simpler molecules. It could also be that the patients produce enzymes that are not working effectively.
Over time,mucopolysaccharides accumulate in connective tissues, cells, blood, the brain, and the spinal cord. As a result, the patient’s appearance, physical ability, organ, system functioning, mental development are all affected.
Mucopolysaccharidoses patients are characterized as short-statured and have tight joints, particularly in the hands.
What are the symptoms of mucopolysaccharidoses?
Symptoms include damage to neurons (which send and receive signals in the body) and pain, corneal clouding, and reduced motor function. This occurs when nerves or nerve roots in the spinal cord or peripheral nervous system are compressed.
Patients may:
- Have normal intellect or be severely impaired
- Experience developmental delay
- Have behavioral issues
It all depends on the type of mucopolysaccharidoses.
What are the orthopedic conditions observed in patients with
mucopolysaccharidoses?
The following are some of the most common orthopedic issues seen in
patients with mucopolysaccharidoses:
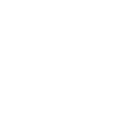
Kyphosis
The primary orthopedic condition of mucopolysaccharidoses is thoracolumbar kyphosis or the gibbus deformity. Gibbus deformities occur in nearly all patients with severe mucopolysaccharidoses I and are commonly found in other mucopolysaccharidoses types as well.
The kyphosis arises from poor bone growth in the anterior–superior region of the cranial lumbar vertebrae. It results in anterior wedging, retrolisthesis of the apex vertebrae and anterior herniation of the intervertebral discs at the thoracolumbar junction.
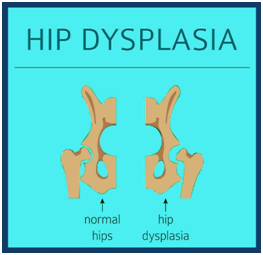
Hip dysplasia
In mucopolysaccharidoses related hip dysplasia there is a poorly development in acetabulum, underdevelopment of the medial portion of the proximal femoral epiphysis and coxa valga. This combination of bone disorders results in hip instability and late dislocation.
This limits the functions when the patient reaches adolescence and early adulthood. Significant hip dysplasia is found in nearly all patients with Hurler and can also be found in patients with attenuated mucopolysaccharidoses I, II, III, IV and VI.
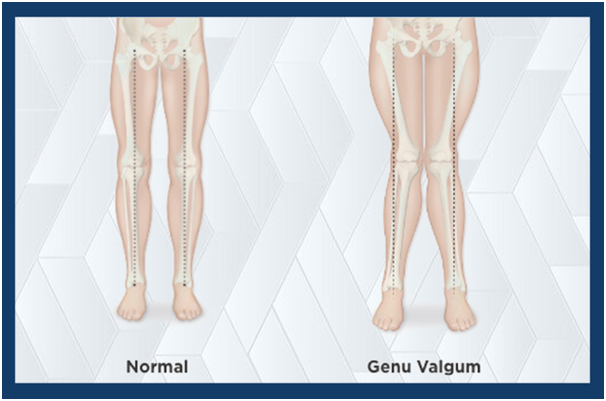
Genu valgum
Almost all children with mucopolysaccharidoses IV, and less than 50% of children with mucopolysaccharidoses I, develop genu valgum or knock kness. Children with mucopolysaccharidoses VI, as well as the attenuated forms of mucopolysaccharidoses I, can also develop valgus deformity severe enough to require surgery.
Some other orthopedic conditions include:
- Problems with the upper cervical spine
- Trigger fingers and carpal tunnel syndrome
How is mucopolysaccharidoses diagnosed?
The first step in diagnosing mucopolysaccharidoses is clinical examinations and pathological tests. These examinations help in detecting excessive mucopolysaccharide excretion in the urine.
To provide a definitive diagnosis, enzyme assays that test a range of cells or blood in culture for enzyme deficiency are required.
Amniocentesis and chorionic villus collection can be used to confirm whether a fetus is affected by the condition during pregnancy.
How are mucopolysaccharidoses treated?
Currently, there is no cure for these diseases. The goal of medical care is to treat systemic diseases and improve a person’s quality of life.
Surgery can help remove excess cerebrospinal fluid from the brain and relieve
pressure on nerves and nerve roots caused by skeletal and other abnormalities.
Corneal transplants can help patients with substantial corneal clouding see better. Tonsillectomy and adenotonsillectomy can help patients with obstructive airway disease and sleep apnea breathe better. An endotracheal tube can also be inserted surgically in some patients to help them breathe.
Enzyme replacement therapies are currently in use for some forms of mucopolysaccharidoses. During enzyme replacement treatment, an intravenous solution containing an enzyme that is defective or missing in the body is used. It does not cure the disease’s neurological symptoms, but it has been shown to help with non-neurological symptoms, including pain.
Bone marrow transplantation (BMT) and umbilical cord blood transplantation (UCBT) have had mixed results in the treatment of mucopolysaccharidoses. Abnormal physical traits can be improved except for those affecting the skeleton and vision. However, this treatment has not proven to be effective for neurological conditions. BMT and UCBT are high-risk treatments that are normally carried out only after intensive evaluation and counseling for family members.
Most orthopedic conditions caused by mucopolysaccharidoses can be improved with the treatments mentioned below
-
Treatment for Kyphosis
Surgery for kyphosis can be required in children as young as two years old, and usually before they reach adolescence. For kyphotic abnormalities, anterior and posterior fusion is suggested, followed by 3–6 months of post-operative bracing. The need for surgery varies depending on the child’s needs and the family’s wishes. In general, a kyphosis of more than 70 degrees are considered relative reasons for surgery
-
Treatment for hip dysplasia
Progressive hip dysplasia can be treated surgically with femoral and pelvic osteotomies. Most children with MPS I eventually require corrective hip surgery. Hip surgery is not recommended in MPS III or VI because of the development of femoral head osteonecrosis. The surgery is easier to conduct at a younger age (around the age of 5–7 years), when the triradiate cartilage is still flexible. Successful surgery becomes more difficult at older ages because of triradiate cartilage closure and permanent femoral head deformation,
-
Treatment for genu valgum
Treatment of genu valgum or knock knees is individualized, but guided growth can be performed in younger patients. In older patients, tibial or fibular osteotomy may be required. As the valgus deformity tends to be focused within the tibia, gradual correction using an external frame is recommended to avoid iatrogenic peroneal nerve palsy.
Some other treatment options include:
- Spine fusion is usually required for progressive abnormalities. Due to hypoplastic spinal components, simultaneous anterior-posterior fusions with instrumentation and protective postoperative bracing may be beneficial.
- Open carpal tunnel release with tenosynovectomy is suitable for carpal tunnel syndrome.
Apart from the treatments mentioned above, physical therapy and exercises can help alleviate joint pain and increase mobility.
Dr.Ratnav Ratan is an expert pediatric orthopaedist practicing in Gurgaon and Delhi NCR offering comprehensive treatment of orthopaedic disorders due to mucopolysaccharide in infants and growing children. These children exhibit skeletal abnormalities very early and hence suitable medical intervention is advisable without further delay.
Also common are hip dysplasia, genu valgum and, later in the course of the disease, spinal cord compression, which can be life-threatening. Short stature is ubiquitous. Treatment of skeletal manifestations usually involves surgical intervention.
Regular imaging of the cervical, thoracic and lumbar spine, the hips and the lower extremities is recommended for patients with MPS.
Skeletal abnormalities are an early and prominent feature of most mucopolysaccharide (MPS) disorders, with the degree of skeletal involvement varying between and within MPS subtypes. Most patients exhibit a constellation of radiographic abnormalities known as dysostosis multiplex, consisting of abnormally shaped vertebrae and ribs, enlarged skull, spatulate ribs, hypoplastic epiphyses, thickened diaphyses and bullet-shaped metacarpals. Thoracolumbar kyphosis or the gibbus deformity is often a key diagnostic clue. Also common are hip dysplasia, genu valgum and, later in the course of the disease, spinal cord compression, which can be life-threatening. Short stature is ubiquitous. Treatment of skeletal manifestations usually involves surgical intervention. All patients with MPS should be considered at high risk for surgical intervention requiring anaesthesia because of airway and cardiac disease manifestations. Regular imaging of the cervical, thoracic and lumbar spine, the hips and the lower extremities is recommended for patients with MPS.